Research Program

Leadership
Keith Nuechterlein, PhD
Director
Kenneth Subotnik, PhD
Associate Director
Contact Info
Aftercare Research Program Website
300 UCLA Medical Plaza
Rm 2240
Los Angeles CA
(310) 206-3142
About
The Aftercare Research Program at UCLA focuses on early intervention and long-term treatment strategies for individuals recovering from a first episode of psychosis. The program combines clinical services with research, aiming to reduce relapse and improve recovery in schizophrenia and related disorders. Areas of focus include cognitive deficits, stress management, and medication adherence. Its work has significantly advanced understanding of early psychosis and effective, evidence-based treatment approaches.
Treatment
When you join the Aftercare Research Program, you will be assigned one of the following psychologists – Dr. Yurika Sturdevant or Dr. Paige Bakman. Your psychologist will be your contact person at the Aftercare Research Program. She will help you coordinate your treatment program activities and develop skills for coping with your daily life. Usually, your psychologist will also be the person who can provide individual therapy or counseling. Upon joining the UCLA Aftercare Research Program, you will be seen once a week through Zoom for your treatment. After 1-3 months, you will be seen twice a week. Family sessions can be scheduled as needed to make sure that your treatment is a “partnership” effort among you, your family, and the Aftercare Research Program clinicians.
You will need to continue taking medication to help you recover from your symptoms and to prevent their return. Your psychiatrist, Dr. Michael Zito or Dr. Dennis Galeano will see you on a weekly or every other week basis, prescribe your medication, and monitor your care. It will be very important that you continue to take your medication regularly
Some aspects of your treatment here will be determined by the research program.
All participants will receive training using specialized computer programs that challenge the brain to improve and grow. These programs help people to improve cognitive abilities, such as memory, concentration, reasoning skills, and ability to learn new things. Social support and self-help materials available only to study participants are provided on-line. As part of our ongoing research protocol, half of the participants will be assigned at random to also receive aerobic exercise classes and exercise homework. Exercise should benefit your physical health and might also benefit your cognitive abilities.
The psychotic disorder that you are experiencing can be best treated when there is a strong partnership among participants, professionals, and family. We feel that young people who experience psychosis can recover best when all elements of this partnership work together in the treatment and rehabilitation process. Thus, we ask that you allow us to discuss your care with your family members as needed to maintain a coordinated treatment plan.
Research Goals

The Aftercare Program is studying ways to improve recovery for individuals with schizophrenia and related disorders, and to overcome challenges that might get in the way of full recovery. We are studying a number of approaches to help patients recover, including cognitive training and exercise.
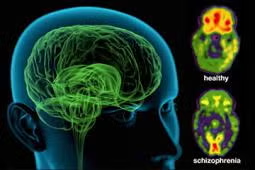
In order to track progress during treatment, we use a number of different types of assessments, some in-person and some remote, including symptom and functioning measures, neurocognitive and social cognitive assessments, psychophysiological measures. . Research assessment batteries are conducted every 3 to 6 months throughout the 12 months of treatment. Our participants are compensated $25/hour for the time they spend completing these assessment batteries. Some assessments may include an MRI brain scan.

The assessments are used in several research projects that are designed to find out more about the symptoms and problems that brought our participants to psychiatric treatment, how these factors influence recovery from these problems, and how they change as the participants challenge their brains to improve as part of their cognitive training. We also use these research assessments to help us gain a better understanding of the role that the brain plays in attention, learning, and memory in schizophrenia and related disorders. We will also learn more about how people with schizophrenia process interpersonal and emotional information, and how that might be related to how well they are doing in their everyday life.
Participants will also regularly be asked about their symptoms and how they are getting along with others. This is a routine part of receiving treatment at the Program.
Who can participate?
Individuals come to Aftercare with unique personal histories and diverse circumstances. The information shared in these interviews will remain confidential, regardless of your eligibility status.
Generally, individuals and/or their loved ones are invited for an intake interview to see if they meet the following criteria:
- Ages 18 to 45
- Experiencing, or have recently experienced, psychotic symptoms including any of the following:
- Hallucinations
- Delusions
At our intake interview, professional staff will speak with you to determine your eligibility for the current research studies. The intake interview will be conducted through a secure internet video connection.
If you believe you or a loved one meets these requirements and would like to learn more, please contact us to request more information or schedule an intake interview.
FAQ
How will the Aftercare Research Program help participants return to school and/or work?
Our therapists/case managers and treatment team members meet with our participants on a weekly basis to discuss goals, and provide support for returning to school or work. We help participants identify schools and/or educational programs that best fit their goals, assist with planning course schedules, study schedules and tips, and assist with academic resources participants may need to acquire (e.g., tutor). For participants who choose to work instead of returning to school, we will assist them with identifying employment opportunities, assist with resumes, role-playing interviews, and aid in the application process.
What can I do if my family member does not want to talk or leave the house?
We understand that communication can be challenging when a loved one is struggling. In some cases, your loved one may not be able to communicate the way you are accustomed to, or may be experiencing symptoms that create difficulties with trusting others. As part of our treatment plan, we provide family education on ways to engage and connect with your loved one, even during some of the most challenging times. Remember that your loved one is going through a difficult time, and for everyone, reassurance goes a long way. Remind your loved one that they can talk with you, or someone that they trust, and that they have support. Encourage them to express their feelings, experiences or concerns. If someone is experiencing hallucinations or delusions, this can feel frightening and your loved one may also be afraid of sounding odd or being judged. Remind them that staying in treatment for their disorder is integral to feeling better. Making empathic statements that convey understanding and compassion rather than exhibiting fear or judgment can facilitate communication. Sometimes finding a joint activity that is comforting can be helpful. For example, taking a walk, or simply sitting together.
What do I do when my loved one refuses to take medication?
Lack of insight and awareness of the need for treatment frequently occurs in psychotic disorders. It is often difficult to understand the need for medication when one does not believe there is an illness or problem that requires treatment. We provide information to participants from an educational standpoint, encouraging them to focus on goals and ways that treatment can allow them to continue to pursue their goals and independence. We also provide psychoeducation and reading materials for family members and loved ones regarding ways to communicate about these difficult topics. One recommended reading is the book, “I’m Not Sick, I Don’t Need Help!,” by Dr. Xavier Amador: http://dramador.com/books/
What are common symptoms of psychosis?
A combination of hallucinations, delusions, or formal thought disorder (conceptual disorganization).
Do participants have to be experiencing psychosis to be eligible?
Aftercare is focused on individuals whom have recently begun experiencing psychosis, however there are other eligibility criteria. If you believe you or a loved one has recently/ is currently experiencing the above symptoms, contact us to inquire about an intake interview.
What does the assessment process look like and how is eligibility determined?
The intake assessment involves an interview that typically takes 2-3 hours long through a secure internet video connection. These assessments help us understand the problems you’re experiencing. Additionally, the intake process requires permission to review your medical records. If you are interested in the treatment provided here, please visit the treatment page.
Is it possible to receive treatment from other clinics/programs concurrently?
Yes, you can see outside therapists or specialists so long as it is coordinated with our program. At Aftercare, we require that you see our in-house Psychiatrist to monitor your medication and well-being.
What is the time commitment for the program?
After an initial period of getting accustomed to treatment, our treatment program will be full days on Tuesdays/Thursdays. After six months, that will change to one day a week. The total duration of treatment is 12-18 months
Do I have to stay on medication?
Medications are a crucial and necessary part of your recovery. While you or your loved one do not have to be on medication to enter the program, taking medication while enrolled in the program is essential. Throughout the program, participants will meet with their Psychiatrist regularly to adjust medication if necessary.
Media Attention
Meet the Staff
-

Keith Nuechterlein, PhD
Director -

Kenneth Subotnik, PhD
Associate Director -

Michael Zito, MD
Psychiatrist -

Dennis Dacarett Galeano, MD, MPH
Psychiatrist -

Joseph Ventura, PhD
Director of Cognitive Training -

Yurika Sturdevant, PsyD
Psychologist -

Paige Bakman, PsyD, LMFT
Psychologist -

Rebecca Zornitsky, MSc
Community Liaison and Intake Coordinator -

Fe Asuan
Senior Administrative Analyst -

Alma Munguia
Patient Coordinator -

Emily McGraw
Neuropsychological Assessor
Gifting
The Challenge
In order to maximize recovery, it is imperative for researchers to implement clinical interventions at early stages of Schizophrenia and related disorders. Therefore, at the Aftercare Research Program, we strive to expand the research base, knowledge, and appropriate treatment methods. Our participant engagement fuels our learning and drives our accomplishments.
The Impact: How does your gift help?
As research on Schizophrenia and related disorders progresses, we hope to improve our methods and quality care for our participants as well. Your contribution would go directly towards providing the highest quality care for our participants’ well-being such as computers for cognitive training, exercise equipment, and pilot study costs.
Participant engagement makes it possible for Aftercare to contribute to treatment and research. In turn, we strive to allocate the best resources for them.
You may make a gift by contacting:
Amy Drizhal
Senior Director of Development, Neuroscience
UCLA Health Sciences Development
10889 Wilshire Boulevard, Suite 1200
Los Angeles, CA 90024
(310) 773-7436
ADrizhal@mednet.ucla.edu

Affiliated